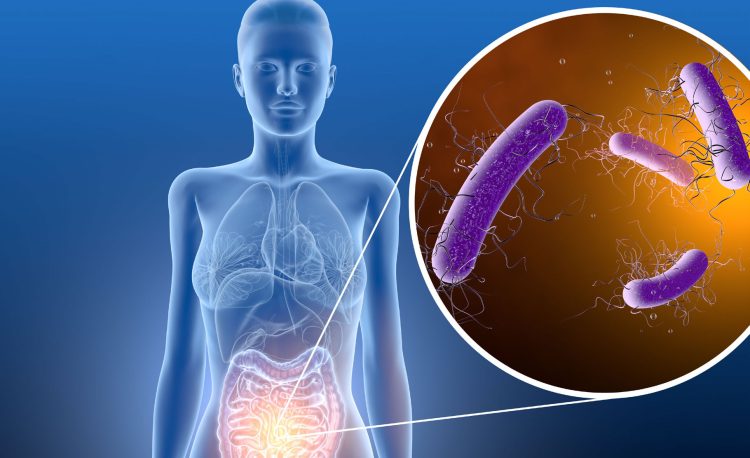
Clostridioides difficile infections The bacterium Clostridioides difficile (C. difficile) causes infectious diarrhea and pseudomembranous colitis. C. difficile infection (CDI) results from the use of broad-spectrum antibiotics, which disrupt the intestinal microbiota, allowing it to proliferate (26), and is the most frequent cause of healthcare-associated infectious diarrhea (27). C. difficile produces two major toxins considered to be primarily responsible for its virulence and the main contributors to its pathogenesis (28). It is disseminated by direct contact between people and contaminated surfaces with high contact potential, both in healthcare establishments and in the community (29) (30) (31).
CDI is generally treated with vancomycin, metronidazole or fidaxomicin as second-line therapy (32). C. difficile is resistant to many antibiotics such as tetracyclines, erythromycin, clindamycin, penicillins, cephalosporins and fluoroquinolones, which are commonly used in the treatment of bacterial infections in the clinical setting (33) (34). The C. difficile genome contains a plethora of mobile genetic elements, which are transferable between C. difficile strains or between C. difficile and other bacterial species, facilitating the spread of antimicrobial resistance (35).